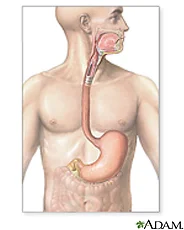
As I explained in last week's blog, the thyroid system plays a critical role in your metabolism. Along with insulin and cortisol, your thyroid hormone is one of the big three hormones that control your metabolism and weight.
The key is the right testing to confirm that a sluggish thyroid is contributing to a stalled metabolism and other problems. Once you know this for sure there are many ways to help correct thyroid problems.
There are so many reasons for low thyroid function, yet I see many patients whose doctors have ignored this problem. One young female patient had more than 30 percent body fat and was unable to change her body no matter how hard she worked. She ate perfectly, exercised with a trainer every day, yet her body wouldn't budge. She also had a slightly depressed mood and other vague symptoms.
I treated her with a low dose of a natural thyroid replacement.
What happened?
Well, she lost 20 pounds and improved her body composition and mood. And all of her other symptoms went away.
How did I know she and other patients had low thyroid function? I ask about symptoms, perform a physical exam, and consider potential causes of thyroid problems. Then I do the right tests.
Most doctors just check something called thyroid-stimulating hormone (TSH), which doesn't give a full picture of the thyroid. In fact, even the interpretation of this test is incorrect most of the time.
The newer guidelines of the American College of Endocrinology consider anybody with a TSH level over 3.0 as hypothyroid. (1) Most doctors think that only anything over 5 or 10 is worth treating. Unfortunately, this leaves millions suffering unnecessarily.
Besides TSH, Functional Medicine practitioners perform other essential tests including free T3, free T4, and thyroid antibodies. We also look for associated problems such as gluten intolerance, food allergies, and heavy metals, as well as deficiencies of vitamin D, selenium, vitamin A, zinc, and omega-3 fats.
Last week I provided some strategies to address underlying causes of hypothyroidism. Here, I want to dive a little deeper to address some strategies to heal your thyroid.
Correcting these problems requires an integrative approach. It involves more than simply taking a thyroid pill. As you'll see, it involves nutritional support, exercise, stress reduction, supplements, reducing inflammation, and sometimes eliminating certain foods and detoxification from heavy metals (such as mercury and lead) and petrochemical toxins (such as pesticides and PCBs).
To integrate all of these elements and create a successful set of techniques to cope with your thyroid problems, I recommend these six strategies.
Strategy 1: Eliminate the causes of thyroid problems.
Carefully consider things that may interfere with your thyroid function and eliminate them. As you will see, there are a good many things that can impede optimal thyroid function.
Diet is a good place to begin. Certain foods have developed a reputation for playing a role in thyroid dysfunction, but this reputation isn't necessarily connected to the latest scientific evidence.
For instance, soy foods and the broccoli family (broccoli, cabbage, kale, Brussels sprouts, and collard greens) have all been linked to thyroid dysfunction, but they also have many other health benefits. Research on these foods to date has been less than conclusive. In one study, rats fed high concentrations of soy had problems with their thyroid. The take-home message: If you are a rat, stay away from tofu. Human studies have shown no significant effect when soy is consumed in normal quantities. (2)
On the other hand, there are food groups where substantive evidence supports a link to an autoimmune disease of the thyroid that slows down your metabolism.
Gluten is one of them. (3) If you think you are having a thyroid problem, you need to do a blood test to identify any hidden reaction to gluten found in wheat, barley, rye, oats, kamut, and spelt. Gluten sensitivity or allergy can cause many different types of symptoms, from migraines to fatigue to weight gain.
Besides doing the blood test, you can simply eliminate gluten from your diet for three weeks. If your symptoms go away, you have a clue that your system might not like this food. If you want to take this self-test a step further, reintroduce gluten into your diet and see if your symptoms recur. If they do, that is another major clue.
There are other food allergies besides gluten that can stall thyroid function. You might want to work with a medical practitioner to pinpoint and eliminate these food allergies. A good place to begin is my book The Blood Sugar Solution 10-Day Detox Diet.
Besides certain foods and food allergies, toxins can slow down your thyroid. Testing yourself for mercury and getting it out of your system and your environment becomes crucial. (4) You also want to avoid fluoride, which has been linked to thyroid problems, (5) and chlorinated water.
Checking for pesticides is more difficult, but supporting your body's detoxification system by eating organic foods, filtering your water, and eating detoxifying foods can be very helpful to heal your thyroid.
Stress also affects your thyroid function negatively. Military cadets in training who were subjected to intense stress had higher levels of cortisol, higher inflammation levels, reduced testosterone, higher TSH, and very low T3. Treating the thyroid without dealing with chronic stress can precipitate more problems.
A common form of chronic stress -- adrenal gland exhaustion or burnout -- particularly becomes dangerous for hypothyroidism. Adrenal gland exhaustion occurs when your adrenal glands are unable to keep up with the physiological needs created by stress.
To remedy this chronic stress, incorporate what I call active relaxation. You might also consider my UltraCalm CD to melt away stress and anxiety.
Strategy 2: Regular Exercise and Saunas
Exercise stimulates thyroid gland secretion and increases tissue sensitivity to thyroid hormones throughout the body. Ideally, you will want to sweat, and the exercise should be vigorous. Regardless of your current fitness level, you will find a helpful, easy-to-implement workout plan here.
Besides being an excellent way to relax your muscles and your mind, saunas or steam baths are a good way to flush your system of pesticides that could be contributing to your thyroid problem.
Saunas are an important aid to weight loss and thyroid repair because as you lose weight, fat tissue releases stored toxins such as PCBs and pesticides (organochlorines). (6) These toxins lower your T3 levels, consequently slowing your resting metabolic rate and inhibiting your fat-burning ability. (7)
Detoxifying becomes an important part of improving your thyroid function. If you don't detoxify, your ability to lose weight decreases as you lose weight because of the released toxins' detrimental impact on thyroid function.
Strategy 3: Eat Foods That Provide Nutritional Support for Your Thyroid, and Avoid Those That Don't
Every step on your road to healing and weight loss depends on proper nutrition and using food to communicate the right information to your genes. (8) Treating your thyroid is no exception.
Choose foods that offer nutritional support for your thyroid. The production of thyroid hormones requires iodine and omega-3 fatty acids; converting the inactive T4 to the active T3 requires selenium; and both the binding of T3 to the receptor on the nucleus and switching it on require vitamins A and D, as well as zinc. You will find these nutrients in a whole-food, clean, organic diet. To get therapeutic levels of these nutrients, please use the supplement protocol in strategy 4.
Thyroid-boosting foods include seaweed and sea vegetables, which contain iodine. Fish (especially sardines and salmon) contains iodine, omega-3 fats, and vitamin D. Dandelion, mustard, and other dark leafy greens contain vitamin A. Smelt, herring, scallops, and Brazil nuts contain selenium.
You want to avoid foods that can interfere with thyroid function. These include the aforementioned gluten. Also, choose clean sources of soy protein in moderation and avoid processed soy products.
Strategy 4: Use Supplements That Support Your Thyroid
Key nutrients for healthy thyroid function are included in my basic supplement recommendations, including a multivitamin and mineral supplement that contains selenium, iodine, zinc, vitamins A and D, and omega-3 fats (fish oil). You will find all these nutrients at my store, as well as a thyroid support kit.
One warning is that if your adrenal glands are burned out from long-term stress, treating the thyroid without supporting the adrenal glands through relaxation and adaptogenic herbs (such as ginseng, rhodiola, or Siberian ginseng) can actually make you feel worse.
I also recommend working with an experienced practitioner who can address individual nutrient needs for your thyroid and, if necessary, also your adrenal glands.
Strategy 5: Have Your Thyroid Tested
There is no one perfect way, no one symptom nor test result, that will properly diagnose low thyroid function or hypothyroidism. The key is to look at the whole picture -- your symptoms and your blood tests -- and then decide.
Doctors typically diagnose thyroid problems by testing your TSH levels and sometimes your free T4 level. But some doctors and clinicians have brought the "normal" levels of those tests into question.
The diagnosis of "subclinical" hypothyroidism that I discussed last week depends on having a TSH level higher than 5 m IU/ml and lower than 10 m IU/ml. As I mentioned above, new guidelines suggest anything over 3 is abnormal. While an improvement, practitioners following these guidelines may still miss many people who have normal test results and a malfunctioning thyroid system.
To get a complete picture, I recommend looking at a wider range of functions:
- Thyroid-stimulating hormone (TSH), the ideal range is between 1 and 2 m IU/ ml.
- Free T4 and free T3 (the inactive and the active hormone).
- Thyroid antibodies (TPO), looking for an autoimmune reaction that commonly goes undiagnosed if the other tests are normal, as doctors don't routinely check this.
- Thyroid-releasing hormone (TRH) stimulation test.
- A 24-hour urine test for free T3, which can be helpful in hard-to-diagnose cases.
A physician experienced in ordering these tests and interpreting the results can provide a more comprehensive picture of how your thyroid is functioning.
If you think you have an undiagnosed thyroid problem, insist that your doctor perform these tests or find a doctor who will. They are essential to fill in the pieces of the puzzle standard tests don't provide.
Strategy 6: Choose the Right Thyroid Hormone Replacement
Ultimately, to properly balance a thyroid that is severely out of balance, you will need to go on some type of thyroid hormone replacement therapy.
Altering your diet and your lifestyle will certainly help tremendously, but if your thyroid isn't functioning properly, you may need to take some additional thyroid hormones to supplement its output. Knowing what's available and what to ask about can empower you to make better decisions about your health.
When I went to medical school and did my residency, I learned about only one treatment for low thyroid function: a synthetic form of T4 that wasn't FDA-approved until recently.
Why do doctors prescribe it? Because that is all they learn to prescribe. But that doesn't make it the best treatment for everyone. Some people benefit from Synthroid, but in some cases the symptoms don't seem to go away using only T4, even if their tests return to normal. So what is the right treatment?
The answer is, it depends.
Part of the beauty (and the headache) of Functional Medicine is that no one treatment works for everyone. A combination of experience, testing, and trial and error becomes necessary to get any treatment just right.
At the same time, I've discovered the majority of my patients benefit from a combination hormone treatment including both T4 and T3. Synthroid is just T4, the inactive hormone. Most doctors assume that the body will convert it to T3 and all will be well.
Unfortunately, pesticides, stress, mercury, infections, allergies, and selenium deficiencies can block that process. Since 100 percent of us have pesticides stored in our bodies, we will all likely have some problem with Synthroid.
The most common treatment I use is Armour thyroid, (9) a prescription drug made from desiccated (dried) porcine thyroid. It contains the full spectrum of thyroid hormones, including T4, T3, and T2 (10). That last one -- T2 -- is a little-known product of thyroid metabolism that actually may be very important. The right dose ranges from 15 to 180 milligrams, depending on the person.
Many doctors still hold the outdated belief that the preparation is unstable and the dosage difficult to monitor. That was true with the old preparation of Armour, not the new one. (See www.armourthyroid.com for more information.)
Sometimes the only way to find out if you have a thyroid problem is a short trial of something like Armour thyroid for three months. If you feel better, your symptoms disappear, and you lose weight, it's the right choice. Once started, you needn't take it for life.
Sometimes, once all the factors that disturbed your thyroid function have been corrected, you may be able to reduce or discontinue the dose. As with any treatment, always work with a physician experienced in using medications to treat your thyroid.
Careful monitoring is essential. Taking too much thyroid hormone or taking it if you don't need it can lead to undesirable side effects, including anxiety, insomnia, palpitations, and, over the long term, bone loss.
Conclusion
Over my several decades working as a Functional Medicine doctor, I can assure you that even in the toughest cases, you can heal your thyroid. With some patients, I can do this through the dietary, nutrient, and lifestyle factors I've discussed here. For others, that healing requires trial and error using several medications and working closely with a physician.
The bottom line is that you should never lose hope. Taking a proactive approach and working with a trained practitioner can correct many thyroid issues.
If you've ever had a sluggish thyroid or other thyroid issues, I encourage you to join our upcoming 10-Day Detox Diet Challenge which will have a bonus segment on Thyroid. Receive a free Ebook, an additional 30 minute live call with a nutritionist, extra coaching support, and my 7-step plan for reversing Hypothyroidism. Click here to register by June 18.
Wishing you health and happiness,
Mark Hyman, MD.
Mark Hyman, M.D. believes that we all deserve a life of vitality -- and that we have the potential to create it for ourselves. That's why he is dedicated to tackling the root causes of chronic disease by harnessing the power of Functional Medicine to transform healthcare. He is a practicing family physician, a nine-time #1 New York Times bestselling author, and an internationally recognized leader, speaker, educator, and advocate in his field. He is the Director of the Cleveland Clinic Center for Functional Medicine. He is also the founder and medical director of The UltraWellness Center, chairman of the board of the Institute for Functional Medicine, a medical editor of The Huffington Post, and has been a regular medical contributor on many television shows including CBS This Morning, the Today Show, CNN, The View, the Katie Couric show and The Dr. Oz Show.
References
(1) Cooper DS. Subclinical Hypothyroidism. NEJM. 2001 Jul 26;345: 260- 265.
(2) Persky VW, Turyk ME, Wang L, Freels S, Chatterton R Jr, Barnes S, Erdman J Jr, Sepkovic DW, Bradlow HL, Potter S. Effect of soy protein on endogenous hormones in postmenopausal women. Am J Clin Nutr. 2002 Jan; 75( 1): 145- 153. Erratum in: Am J Clin Nutr. 2002 Sep; 76( 3): 695
(3) Toscano V, Conti FG, Anastasi E, Mariani P, Tiberti C, Poggi M, Montuori M, Monti S, Laureti S, Cipolletta E, Gemme G, Caiola S, Di Mario U, Bonamico M. Importance of gluten in the induction of endocrine autoantibodies and organ dysfunction in adolescent celiac patients. Am J Gastroenterol. 2000 Jul; 95( 7): 1742-1748.
(4) Ellingsen DG, Efskind J. Effects of low mercury vapour exposure on the thyroid function in chloralkali workers. J Appl Toxicol. 2000 Nov- Dec; 20( 6): 483- 489.
(5) Galletti PM, Joyet G. Effect of fluorine on thyroidal iodine metabolism in hyperthyroidism. J Clin Endocrinol Metab. 1958 Oct; 18( 10): 1102- 1110.
(6) WJ, Pan Y; Johnson AR, et al. Reduction of chemical sensitivity by means of heat depuration, physical therapy and nutritional supplementation in a controlled environment. J Nutr Env Med. 1996;6: 141- 148.
(7) Pelletier C, Imbeault P, Tremblay A. Energy balance and pollution by organochlorines and polychlorinated biphenyls. Obes Rev. 2003 Feb; 4( 1): 17- 24. Review.
(8) Bland J. Nutritional Endocrinology, Normalizing Hypothalamus-Pituitary-Thyroid Axis Function, 2002 Seminar Series Syllabus.
(9) Gaby AR. Sub-laboratory hypothyroidism and the empirical use of Armour thyroid. Altern Med Rev. 2004 Jun; 9( 2): 157- 179.
(10) Goglia F. Biological effects of 3,5-diiodothyronine (T( 2)). Biochemistry (Moscow). 2005 Feb; 70( 2): 164- 172.